Revenue Cycle Management
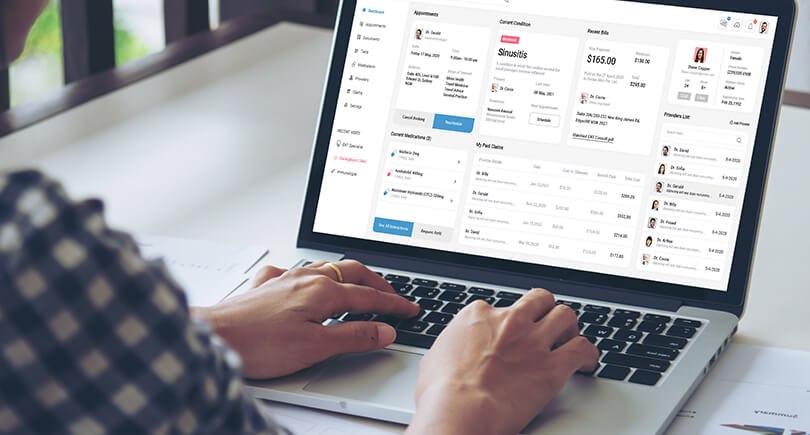
At Physicians Revenue Cycle Management we bring a time-and-process-optimized AI solution forth for our clients. Facilitating an end-to-end billing process across specialties from the creation of a claim to submission of the claim to the automated follow-ups, from denial management to payment appeals, posting and reporting.
Our Fore-Fronts
The implementation of an effective RCM process is critical to the financial health of healthcare organizations. By optimizing the revenue cycle, healthcare providers can improve their cash flow, reduce bad debt, and enhance patient satisfaction. RCM is also essential for complying with regulatory requirements and ensuring that healthcare organizations are reimbursed accurately for their services.
Operational Agility
Systemized and Structured Billing Process
Prompt Documentations
Eligibility Verification
Analytical Partner
Visibility Performance Indicators
Practice Revenue Monitors
Routine Patient Diagnostics
Tracking & Followup Agent
Customer-Centric Tracking System
A/R Management
Automated & Rigorous Follow-ups

Patient Registration
Patient registration is the first step on any medical billing flow chart. This is the collection of basic demographic information on a patient, including name, birth date, and the reason for a visit. Insurance information is collected, including the name of the insurance provider and the patient’s policy number, and verified by medical billers. This information is used to set up a patient file that will be referred to during the medical billing process.
Financial Responsibility
The second step in the process is to determine financial responsibility for the visit. This means looking over the patient’s insurance details to find out which procedures and services to be rendered during the visit are covered. If there are procedures or services that will not be covered, the patient is made aware that they will be financially responsible for those costs.


Superbill Creation
During check-in, the patient will be asked to complete forms for their file, or if it is a return visit, confirm or update information already on file. Identification will be requested, as well as a valid insurance card, and co-payments will be collected. Once the patient checks out, medical reports from the visit are translated into diagnosis and procedure codes by a medical coder. Then, a report called a “superbill” may be compiled from all the information gathered thus far. It will include provider and clinician information, the patient’s demographic information and medical history, information on the procedures and services performed, and the applicable diagnosis and procedure codes.
Claims Generation
The medical biller will then use the superbill to prepare a medical claim to be submitted to the patient’s insurance company. Once the claim is created, the biller must go over it carefully to confirm that it meets payer and HIPPA compliance standards, including standards for medical coding and format.


Claims Submission
Once the claim has been checked for accuracy and compliance, submission is the next step. In most cases, the claim will be electronically transmitted to a clearinghouse, which is a third-party company that acts as a liaison between healthcare providers and health insurers. The exception to this rule are high-volume payers, such as Medicaid, who will accept claims directly from healthcare providers.
Monitor Claim Adjudication
Adjudication is the process by which payers evaluate medical claims and determine whether they are valid and compliant, and if so, the amount of reimbursement the provider will receive. During this process, the claim may be accepted, rejected or denied. An accepted claim will be paid according to the insurers agreements with the provider. A rejected claim is one that has errors that must be corrected and the claim resubmitted. A denied claim is one that the payer refuses to reimburse.
Statement Follow-Up
The last step in the medical billing process is to make sure bills are paid. Medical billers must follow up with patients whose bills are delinquent, and, when necessary, send accounts to collection agencies.
Professional Skills
We Have 50+ Winning Awards

Don’t Be Hesitate To
Contact Us
A one-window solution to managing the end-to-end revenue cycle
Book a demo
Call Us: 630-643-1972
84k+
Happy Clents
Our Response To Your Quick Queries
Get Your General Answer
Physicians Revenue Cycle Management is a cloud-based fully automated system designed to facilitate quicker and simpler UX & UIs for our customers.
Depending upon small, medium and large-scale practices Go-Live timeline varies from five (5), eight (8) and ten (10) weeks respectively.
Physicians Revenue Cycle Management is certified by